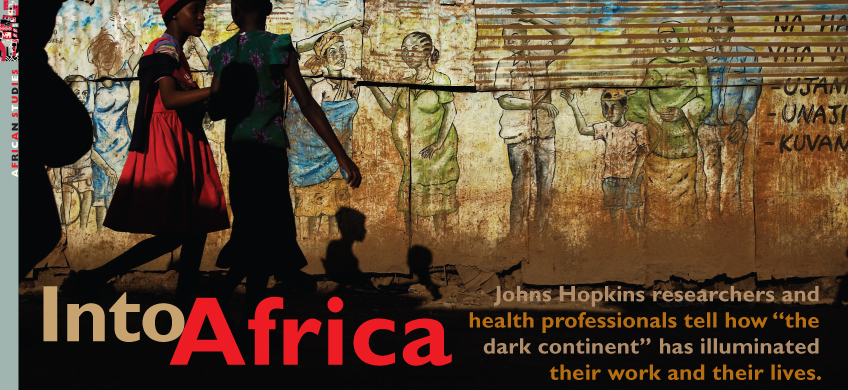
They travel in search of answers, and adventure often finds them.
Hundreds of Johns Hopkins academics, clinical workers, employees, and researchers work in Africa, seeking knowledge about cultures, disease, and the past. They do so at some peril. Before they board a plane, they are vaccinated against yellow fever, hepatitis A, rabies, typhoid, and meningitis. They are prescribed drugs to ward off the continental scourge—malaria—and unrelenting diarrhea caused by local food and water. They often come face to face with political violence, as the case of Stephen Okiria—a Bloomberg School of Public Health employee killed by a terrorist’s bomb earlier this year in Uganda—chillingly proves.
Yet, few have misgivings. The chance to aid a largely impoverished population—the United Nations’ list of the 10 poorest countries worldwide is entirely African—and to fully explore the realm of disease on the continent offers researchers a living laboratory. It’s an opportunity too meaningful to pass up.
Beyond medicine—and the anthropology, Egyptology, and paleontology university researchers investigate there—are the people and places of Africa. Many Westerners who make the trip say that Africa changes them. Much of what they learn has little to do with their discipline, and everything to do with perspective.
“I have learned patience, how dependent the world is on the Internet, how to slow down and appreciate people, and how not to get too frustrated,” says Sara Groves, an assistant professor at the School of Nursing. She has spent the past two years in Kampala, Uganda, as part of a cadre of Johns Hopkins clinicians and researchers from various schools who work to increase the numbers of Ugandan health workers and medical scientists. “I’ve learned just how hard African lives are outside the workplace.”
Inside are five edited interviews with Johns Hopkins people who have either uprooted their comfortable American lives or left middle-class African neighborhoods to work amid the poor, sick, and needy on their native continent. Each tale is a measure of science and soul.
Chad has been the backbone of my career. It’s why I chose to study public health at Harvard, completing my dissertation in the southern part of the country during the 1990s. And oil has always been the backdrop for any conversation on the future of Chad, which ranks 170th out of 177 countries measured by the U.N. Human Development Index. International oil companies began exploring the possibilities for petroleum there in 1969. By the 1990s, they had worked out plans with the Chadian government, which had gotten loans from the World Bank to help finance a pipeline that would stretch from southwestern Chad to Cameroon’s Atlantic coast. I wondered what this huge potential change in the country’s fortunes would mean for people, especially those who live in the oil field region, and who grow millet, sorghum, sesame, and peanuts on the lands around them.
When I came to Hopkins in 2000, I already had in mind exploring oil as a substance that was supposed to improve people’s lives. I’ve spent three to four months each year in Chad since. My plan was to really make this a longitudinal study—about 25 years, what was planned as the life of the oil fields. But the project as “an experiment in development” ended in 2008, when the World Bank pulled out, arguing that the Chadian government had not kept its part of the deal to spend 80 percent of its oil sale proceeds on health, education, and rural development—a “future generations fund.” While I am still doing research in Chad, at this point I’m mostly focused on writing.
The study involves 160 households. I’ve followed the lives of the people in 80 of them, spread across three villages, especially closely. I’ve seen attitudes toward oil and the project change. When the first oil well was capped in the middle of the three villages, people who live there took pride in it—they’d clean around it, cut the grass, and clear the overgrowth. They had been told for years that this was their future. Now, there are security guards all over the place and the wells are off-limits. It’s a completely different relationship.
Oil companies have taken land, offering some cash in return, but they initially underestimated how much the project would need. In one village, 90 percent of people have lost land. Many families have had to learn to make vegetable oil, repair motorcycles, do carpentry work, or vaccinate chickens to try to make up for the loss of land. Most of them haven’t been successful because those jobs they’ve been retrained to do don’t get them enough work. Relocation isn’t an option.
People are disappointed and frustrated. It’s been hard for them to keep up with the changes demanded of them. And the state once had a lot of interest but now limits much of what it does to policing and security.
The very general question I asked when I started this was: How does this kind of “development” work? The bevy of environmental and social regulations and the policies governing the way land was acquired were supposed to serve as a model for other projects of this kind—at least that’s how the government and the World Bank saw it. I investigated how those concepts worked out at the micro level. One of the things I learned was that while it is important for this consortium of oil interests to show that they were adhering to global standards and policy prescriptions, they knew little about the day-to-day lives of people those standards aim to protect and even to help. It was interesting to explore the mundane ways in which people got along in the wake of the project.
I have a lot of friends in Chad—my days there are filled with friends. Here in the States, there’s a lot of time spent alone. There, the norms of sociality are completely different. I’ll spend days talking with people while they work in the fields or make a chair or cook a meal. That kind of closeness, developed over many years, greatly aids the research. But it means so much more than that.
When I first traveled to Mali as a Peace Corps volunteer in the mid-1990s, I spent one of my first nights in a hut during a rainstorm. I was forced to move closer and closer to the center as the mud walls slid in around me during the deluge. Early in the morning, I emerged expecting sympathy and shock from my hosts. All I saw were women busy repairing their homes. They laughed when they saw how distraught I was. It was one of my first lessons in the resiliency and strength of Malian women. When you understand how much they do in terms of raising children, farming, carrying water and wood from long distances—basically moving nonstop from 4 in the morning to past midnight—you forget about whatever complaints you had about your comfortable Western life.

Nicole Warren (far left) started the nonprofit Mali Midwives to help matrones improve their midwifery skills. “They have grown tired of watching mothers and babies die,” she says. Photo Courtesy of Nicole E. Warren
For pregnant women, the work is even more difficult. In Mali, they say a woman has one foot on the earth and the other in the grave. In poor rural areas, where most Malians live, and where hospitals are hours away and transportation is chancy, a woman suffering from a postpartum hemorrhage can bleed to death in a matter of hours. Mali has one of the highest rates of maternal death in the world—nearly one in 200 births—and there are a lot of near misses. Women who survive life-threatening complications often have trouble breastfeeding or helping with the harvest. Their family’s economic future, already fragile, can be devastated.
Midwives are often present during childbirth, but there are too few of them. Fortunately, there are auxiliary midwives called matrones, about 140 of them in Koutiala, a region in Mali’s southeast where about 400,000 people live. For most women, a matrone is the most highly trained provider they’ll ever see. Unfortunately, most matrones are poorly equipped, working by a lantern’s light with nothing more than a black plastic tarp to offer the birthing woman to lie on. They might work with little more than a clamp, old scissors, a bottle of water, some bleach, some cotton, and a bucket. More importantly, for all the great work they do, they aren’t as well trained as they need to be. They are acutely aware of this. They have grown tired of watching mothers and babies die.
I started a charity, Mali Midwives, to understand the challenges matrones face and to help them improve their midwifery skills. Our work has supported the Mali Ministry of Health’s plans to get more priority care training to every level of the health system. The matrones and their supervisors got together and decided what the agenda for their education should be. In the first year, 2008, we updated their skills in essential newborn care. Since then, we’ve concentrated on the third stage of birthing, when the placenta is delivered following a birth. Bleeding during this time is the No. 1 reason women die during childbirth. Mali Midwives coordinated training in which local experts showed matrones a set of simple skills to prevent the uterus from bleeding too much during the third stage.
But there are a lot of things—cultural things—that training can’t really get at. Matrones struggle for respect. Most have low social standing because they are young and female. In the health care system, they can be regarded as country bumpkins because of their links to rural life. When a woman is having problems during childbirth, the matrones face harrowing choices: Should they stay to support the woman? Or do they use precious time to find the village authorities or the woman’s family to arrange transportation—a truck, a donkey cart—to get her to a distant hospital? They often have to navigate the realm of men, where they have no real power. Yet, these women persist in providing reproductive health care along with the usual obligations of farming and family life.
They’ve certainly earned my respect. I’ve remained friends with several during the past 15 years. When my daughter, Felix, was spending the first year of her life in Mali, matrones and other women there began treating me as a woman, and not as an outsider. They critiqued my breast-feeding technique and taught me how to properly tie my child to my back. When you’re a wife and mother, they understand you. They’re more likely to laugh with you.
The grace they show while leading often-difficult lives is inspiring. One of the reasons I keep these pictures of Mali hanging in my office in Baltimore is that it’s so easy to get caught up in the fast-paced Hopkins environment, to get consumed by the work here. The photos remind me of what real work is.
I was born in a Nairobi neighborhood, but the church and school I went to were in the makeshift places built on the edges of our society, the slums. I’ve experienced a lot there, and some members of my family have suffered poor health in part because of the slum environment they lived in.

Jane Otai (left) runs a program that works to improve health care in the slums of Nairobi. “In the slums,” she says, “it’s no different from anywhere else—people want to live a good life.” Photo Courtesy of Jhpiego
It’s intensely crowded in Korogocho and Viwandani—the slums where I now work. Many families live in houses that are no more than 10 feet by 10 feet, with mud-plastered walls and a corrugated metal roof. Houses aren’t ventilated properly, so you see a lot of tuberculosis. There might be a communal toilet. Many have to pay to use it but can’t afford it, so you’ll see people do their business in a plastic bag instead, and then throw it out into the fields. Having all that around leads to high rates of diarrhea, skin disorders, and cholera. There’s a good bit of crime and much unemployment and underemployment, which is a bit ironic given that so many people come to Nairobi from rural areas or Somalia in hope of finding work. Many people make no more than $2 per day. Some women turn to prostitution—one of the reasons why nearly one in seven people here has HIV or AIDS.
I started working with children in the slums more than two decades ago to get more of them into schools. I ran a soup kitchen and founded a training program for youths and parents who needed jobs. I also started a health clinic.
When I was at a conference in Italy in 2005, Pamela Lyman, the director of the Kenyan programs at Jhpiego, Johns Hopkins’ international affiliate that focuses on ways to improve health, heard me speak and hired me to run a program centered on the slums. Since then, we’ve tried to empower people. We teach HIV-infected persons how to handle aspects of their own care by showing them how to regularly use their medicines and get to health facilities in Nairobi. We created a map that shows people where an array of services—clinics, nutrition, schools—is situated. We also train providers of health services, link them to the national health ministry, and make sure they get antiretroviral drugs. We try to help people, especially women, deal with some cultural things. In some communities, it is difficult for women to have the power to tell their men to use condoms, particularly if they’re married.
In the slums, it’s no different from anywhere else—people want to live a good life. When you arm them with education, they have more power to create that life. It once was a challenge to get men involved in issues of health, particularly if they involved women and children. But we’ve managed to get men to rally around health issues, like HIV, reproductive health, water, and sanitation. In Korogocho, we’ve helped support Men’s Movement Against AIDS. Members meet as men and discuss men’s issues, including condom use, how AIDS is transmitted to an unborn child, and family planning. And we’ve provided wheelbarrows, rakes, and the like to young men who decided to gather together and clean up their villages. They don’t want their children to suffer from the usual slum diseases.
Before I joined Jhpiego, I would go into the communities and say things like, “Here’s your problem: Your children don’t get enough nutrition. Here’s how you can solve that.” But working with Jhpiego has taught me that we shouldn’t be dictating to people. Instead we give them training and equipment and get them thinking about how to improve their lives.
Right now, about 40 percent of Nairobi’s population of around 4 million lives in places like Korogocho and Viwandani. By 2030, urban slum dwellers will make up 72 percent of the population in African cities, the United Nations tells us. What I see here is the future, one we need to understand so we don’t have to deal with catastrophes in public health.
I grew up in Sudan, in a bustling place along the Nile. Our great fathers, the Nubians, thought they owned the river. Historically, the Nile Valley has been very active—people coming in and going out—but has offered little in the way of health or educational opportunities. Nonetheless, I was trained to be a physician and practiced for several years in Sudan, working on cases of tropical diseases, such as malaria and schistosomiasis. Epidemics such as meningitis and cholera were very common in many African countries, with people traveling from West Africa to East Africa along the famous “meningitis belt.”
After spending some time in clinical practice in Africa, you realize you have to do more than treat one patient at a time. I became involved in public health because of my interest in doing research that would get at these big African health problems. I got my PhD in public health from Johns Hopkins and traveled to Malawi to begin investigating HIV. In 1992, when I was asked by my superiors at Hopkins to go there, I responded that I would rather go to East Africa, West Africa—anywhere else other than the south of Africa. I knew nothing about the southern part of the continent. What I learned when I got to Malawi was that the cultures in Africa are actually very similar. They have common customs, common diseases, and back then they had little research capabilities to deal with them.
Most of our activity has been built around AIDS in pregnant women and their children. We started looking at what the risk factors were. We learned that having multiple sexual partners and not using condoms were spreading disease. But we also learned that many mothers were infecting their babies during breast-feeding. Currently, about 20 percent of pregnant women are HIV-infected. We developed prevention programs, encouraging people to change their sexual practices.
Most recently, we’ve done several studies and clinical trials to see what we can do to stop HIV transmission via breast milk. We did one trial involving more than 3,000 Malawian babies and found that by giving infants a certain drug regimen, we can protect them from HIV in their mother’s breast milk for up to 14 weeks. We didn’t go further than that at the time because of safety concerns about the effects of the drugs. But now we know that they are safe and we’re looking to give them the regimen for the entire time they are breast-feeding. We’re also looking at ways to give the mother antiretroviral drugs while she’s breast-feeding. These two methods of prevention may be equivalent. You don’t want to give some women these drugs until their immune systems are in dire need of them, so there are some extra considerations there.
My wife and three sons lived with me in Blantyre for five years and they really enjoyed it. We returned to the United States for my sons to continue their education after high school. Otherwise, I’m not too sure that we would have come back. I make several trips back to Malawi each year. The people are warm, friendly, and happy to deal with you. When you do this kind of work, you really feel like you are doing what you need to do. You’re living among the people and doing what you can to help them and their community. You talk to people and help educate them, too. In turn, they honor you by giving you a place there.
When I was told three years ago that there was a chance to study the intersection of tuberculosis and HIV in Africa, I jumped at it. Uganda is really the epicenter of HIV in Africa—the first African case of the disease was diagnosed along the border with the Democratic Republic of Congo in 1982. It’s an infectious-disease scientist’s dream to be where the action is, and HIV is the infection of my lifetime. Ever since I completed my residency at Johns Hopkins in 1994, it has molded my life as a researcher. It has driven me to investigate the possibilities for diagnostic tests and a vaccine for tuberculosis, one of the diseases HIV-positive people are most likely to acquire. So I brought my four boys—now ages 8 through 16—to Uganda, as well as my husband, who now works here as a medical epidemiologist for the Centers for Disease Control and Prevention.

Many Johns Hopkins researchers, including Taha Taha and Yukari Manabe, are working to stop the transmission of HIV in Africa. Photo: David Colwell
When we got here, I was overwhelmed by how green the country is despite being overcrowded, especially in Kampala, the capital. People are warm and speak English here, too, so I began to understand why there were so many retirees from international nonprofits who choose to settle here.
Beyond the beauty and friendliness is a lot of suffering, however. Rates of HIV and its related infections have come down since their peak prevalence in the 1990s, but along with malaria, they still dominate the medical landscape here. It’s hard not to see how difficult the lives of so many Ugandans are. The need is intense. When I worked in the TB clinic in East Baltimore, there might have been 44 total cases we tracked. Here, we’ll see 350 to 400 people in just one clinic. It’s staggering.
I’ve continued my research into TB and have participated in several studies on HIV-associated complications and cryptococcal meningitis, a fungal disease that causes inflammation in the space between the brain and skull; it’s another often-fatal infection that people with HIV contract. At the Infectious Disease Institute, our goal is to increase the numbers of native Ugandans who study medicine and research and then go on to independently conduct research on questions that will change the lives of Ugandans. We rely on local and international faculty to train them. There are five of us from Hopkins living here.
Besides overseeing the work done at the institute, I’ll also travel with some students two and a half hours outside Kampala to oversee clinical trials in a district hospital in Kiboga. People with HIV are much more likely to die from opportunistic infections like TB here than patients in the United States, even if they take antiretroviral drugs. We’re trying to find out why. I’m also running trials to see if we can develop a diagnostic tool for TB that doctors don’t have to administer. One of the methods we’re looking at involves a dipstick that would test urine for the presence of cell wall components that signal the presence of TB.
My level of admiration for people here who live with and treat disease is boundless. The doctors seem to have tireless energy, even though one-third of the people they see in the hospital will die. Many of them have to work without water or power for long stretches of time. They deal with this despite the basic unfairness of life, and somehow maintain the energy to both see patients and conduct research.
I’ve learned how deeply people can care for each other here. When I returned from a recent trip to do clinical research in Mozambique, people said, “Dr. Yuka, you were lost.” What that means is, “We missed you. You were lost, but now we’ve found you. It’s nice to see you.” When I heard sentiments like that when I first got here, I thought it was out of politeness. But now I know that it comes from the uncertainty of life in settings with few resources, and from not knowing what tomorrow will bring. It’s a way of showing people how much you care every day.
Michael Anft is Johns Hopkins Magazine’s senior writer.